Everything You Need to Know About HPV
Welcome to the Sensate Health blog! While I am a physician, this blog is for educational purposes only and does not constitute medical advice or a doctor-patient relationship. Please see your healthcare provider for any medical concerns.
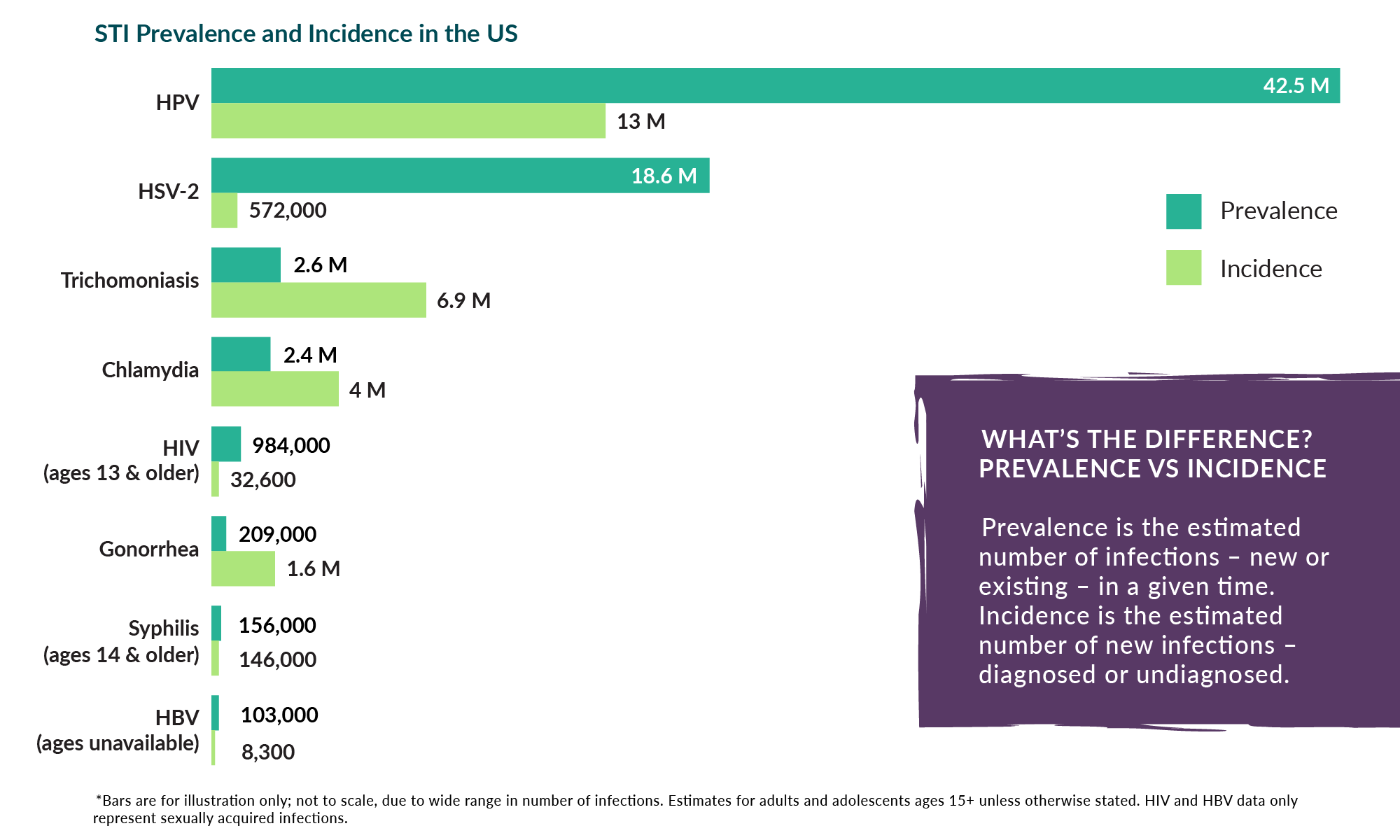
Human Papillomavirus (HPV) is the most common sexually transmitted infection in the world, and an estimated 43 million Americans are currently living with HPV. While the vast majority of HPV infections are asymptomatic and resolve on their own, they can also lead to rare but serious health issues. Furthermore, limitations in how we test for HPV can lead to uncertainty and stress when navigating a new diagnosis with partners. In this post, we will delve into the world of HPV, exploring everything you need to know to navigate an HPV diagnosis or reduce your chance of acquiring a new infection.
What Exactly Is HPV?
HPV is a diverse family of viruses with over 100 known strains. Some are considered high-risk and have the potential to cause cancer (predominantly cervical cancer but also cancers of the genitals, anus, and throat), while others are low-risk and may lead to benign conditions like warts. However, the vast majority of cases are completely asymptomatic (most people never even know about the infection), and 90% of cases resolve on their own within two years. When cancer does occur, it can take years or even decades to develop.
As mentioned above, around 43 million Americans currently have HPV, and an estimated 13 million new infections occur each year. The CDC estimates that about 85% of people will get an HPV infection in their lifetime. HPV does not discriminate based on age or gender. While it's most commonly associated with younger individuals, it can affect people of all ages. Additionally, people of all genders can contract and transmit the virus, making it an important public health issue for everyone.
How is HPV Transmitted and Diagnosed?
HPV is most commonly transmitted through skin-to-skin contact and through sexual contact, including vaginal, anal, and oral sex. Because HPV can be transmitted through contact with skin and not just the genitals, transmission can occur even during safer sex, through contact with areas that aren’t covered by the condom or dental dam. The fact that HPV transmission can’t be eliminated through consistent condom use helps to highlight the importance of vaccination, but we’ll get to that later in the article. Lastly, HPV has been found to persist on the surfaces of sex toys, so shared toy use is another possible means of transmission.
One of the complications in trying to reduce HPV transmission is that it isn’t included in routine screenings for STIs. This is because of limitations in our current testing methods and a lack of health outcomes data to support more widespread screening. For someone with symptoms of an HPV infection, most commonly warts, HPV can be diagnosed through a clinical exam by a healthcare provider. In some cases, the diagnosis may be confirmed with a biopsy.
For those who don’t have any symptoms, pap smears are performed on individuals with a cervix to screen for cervical cancer from ages 21 to 65. From ages 21 to 29, this consists of looking at the cells for any HPV-related precancerous changes, but starting at age 30 the pap smear may also include a test for HPV itself. People who have receptive anal sex should check with their doctor about whether anal cancer screening is recommended for them, especially if they’re living with an HIV infection. There are currently no recommended HPV screenings related to penile cancer, which means the preventive measures below are even more crucial.
What Should I Do if I’m Diagnosed with HPV?
First and foremost, recognize you’re not alone! Most people will get HPV in their lifetime, and most cases resolve on their own without any long-term complications. If you’ve been diagnosed with anogenital warts, talk to your healthcare provider about treatment options to help accelerate your body’s clearance of the infection. This may consist of topical treatments that you can do at home, or your clinician may provide treatments in the office.
If you were diagnosed with HPV on a pap smear, your healthcare provider may recommend monitoring the infection with repeat pap smears, or they may recommend a procedure called a colposcopy. This consists of looking at your cervix with a microscope during a pelvic exam, and they may also collect a biopsy during this procedure to assess their findings in more detail. Most cases of cervical HPV infections can be monitored over time until they resolve on their own, but if the precancerous changes progress, your clinician may recommend a procedure called a LEEP or cone to remove a part of the cervix. This intervention, along with continued monitoring, is highly effective in preventing progression to cervical cancer.
Can you have sex with an HPV diagnosis? Absolutely yes! It’s recommended to tell your partner about your diagnosis so that they can provide informed consent and you can discuss together what protective measures you’d like to take such as condoms or Gardasil vaccination (see information on prevention below). If you have warts or are receiving active treatment for any HPV infection, please check with your healthcare provider before engaging in sexual activity. But don’t forget - even if you need to avoid genital contact while recovering from treatment, there are many other ways to be sexual with your partner.
How Can I Prevent HPV?
Because HPV is so common, the only way to truly prevent infection would be abstinence and essentially avoiding any skin contact with another person. Since that’s not feasible for most people, we’ll talk below about ways to reduce your chance of infection and any subsequent complications.
Gardasil Vaccine
Have you heard that there’s a vaccine that can help prevent cancer? The Gardasil vaccine does just that. Initially covering four HPV strains and now covering nine, including the most common strains that cause anogenital warts and cervical cancer, Gardasil is recommended routinely for children of all genders at age 11 or 12 but can also be given to teens and adults up to age 45 if not vaccinated previously. While most adults will need to get three doses of the vaccine for optimal immunity, research shows that even one dose of Gardasil is highly effective in preventing HPV infection.
It’s important to know that Gardasil doesn’t cover all HPV strains, so it’s still possible to contract HPV despite receiving the vaccine. However, these infections are likely to be with lower-risk strains that may resolve on their own without further intervention. Please follow your healthcare provider’s recommendations regarding follow-up for further testing or treatment. Of note, it is also possible to be infected with more than one strain simultaneously or over the course of a lifetime, and in rare cases a prior HPV infection can reactivate at a later time.
Safer Sex Practices
Practicing safer sex, including consistent condom and/or dental dam use and not sharing toys, can reduce the chance of HPV transmission. However, condoms do not provide complete protection since the virus can spread through skin-to-skin contact on areas not covered by the condom. For some people, practicing mutual monogamy, where you only have sex with someone who also only has sex with you, or otherwise limiting sexual partners can also help reduce the chance of acquiring HPV. While HPV isn’t included in routine STI testing, having conversations about safer sex practices and STI testing is an important part of any strategy to reduce your chances of acquiring a new infection. That being said, the reality is that most sexually active people will acquire HPV at some point.
Screening
Last but certainly not least, if you have a cervix and are between the ages of 21 and 65, it’s important to make sure you’re up to date on your pap smear. While pap smears don’t prevent HPV, they help ensure that the infection isn’t able to progress to the point of causing negative health consequences. If you have receptive anal intercourse, ask your healthcare provider if anal cancer screening is recommended for you, especially if you’re living with HIV.
Conclusion
HPV is an immensely common infection affecting about 85% of individuals at some point in their lifetime. Most cases are asymptomatic and resolve on their own without intervention, but some infections cause warts or precancerous changes and should be treated. HPV testing isn’t included in most routine STI screenings. While HPV isn’t completely preventable among people who are sexually active, there are steps you can take to help protect yourself from the complications of an HPV infection, especially through Gardasil vaccination and cervical cancer screening with pap smears.
If you have questions about your own sexual health, as of the time of this publication you can schedule a free 15-minute coaching consultation with me here.
Here’s a Recap of What We Discussed:
About HPV
Affects about 85% of people
Over 100 strains, generally divided into high-risk types that may progress to cancer and low-risk types that can cause warts
Most cases are asymptomatic and resolve on their own
HPV Transmission and Diagnosis
Transmitted most commonly through sex and skin-to-skin contact
Isn’t included in most routine STI screenings
Warts can be diagnosed on physical exam or may be confirmed with a biopsy
Pap smears detect HPV and related precancerous changes for individuals with a cervix
What to Expect After Diagnosis
Treatment is recommended if warts are present
HPV detected on a pap smear may be monitored on repeat pap smears or investigated further with a colposcopy
You can still have sex after an HPV diagnosis - check with your healthcare provider first if you have warts or are receiving any current treatment
Prevention
Only true way to prevent is abstinence and avoiding all skin contact
Gardasil vaccine can be given up to age 45
Covers the most common strains that cause cancer and anogenital warts but doesn’t cover all strains
Safer sex practices
Condoms/ dental dams - aren’t completely effective since there are still exposed areas for skin-to-skin transmission
Limiting number of partners
Having conversations about safer sex and STI testing
Screening
Cervical cancer screening for people with a cervix between the ages of 21 and 65
To schedule a coaching session with me, click here.